Postpartum Depression vs. Normal Adjustment: How to Tell the Difference
Navigating Postpartum Emotions: What’s Normal and What’s Not
Bringing home a new baby is often described as magical, but for many parents, the experience feels more like a roller coaster of exhaustion, mood swings, and overwhelm. Between sleepless nights, endless feeding cycles, and adjusting to a completely new identity, it’s natural to feel off-balance.
But sometimes the struggle goes beyond "normal adjustment." Postpartum depression (PPD) is a real, common, and treatable condition, and knowing the difference matters. In this blog, we’ll explore what’s expected during postpartum recovery, what’s not, and how to tell when you may need extra support.
What Are Normal Postpartum Adjustment Challenges?
The postpartum period (often called the "fourth trimester") is filled with massive emotional, physical, and hormonal changes. Even in the best circumstances, it’s completely normal to experience:
Mood swings
Fatigue and overwhelm
Increased irritability
Crying spells
Self-doubt about parenting
Feeling disconnected from your pre-baby identity
Why These Normal Adjustments Happen
Adjusting to a newborn is demanding for many reasons:
Hormonal fluctuations: After delivery, estrogen and progesterone levels drop dramatically.
Sleep deprivation: Newborns don’t care about your circadian rhythm.
Identity shifts: You’re suddenly responsible for keeping a tiny human alive.
Physical recovery: Whether vaginal birth or C-section, the body is healing.
These challenges can feel overwhelming but typically improve with rest, support, and time.
What Is Postpartum Depression (PPD)?
Postpartum depression is a clinical condition that affects up to 1 in 7 birthing parents. It’s more intense, longer-lasting, and more disruptive than typical postpartum stress.
Common Symptoms of PPD:
Persistent sadness or emptiness
Loss of interest in activities
Difficulty bonding with the baby
Intense guilt or feelings of worthlessness
Anxiety or intrusive thoughts
Hopelessness
Trouble sleeping even when the baby sleeps
Changes in appetite
Thoughts of self-harm or harming the baby
PPD is not your fault. It’s caused by a mix of hormonal, environmental, and psychological factors.
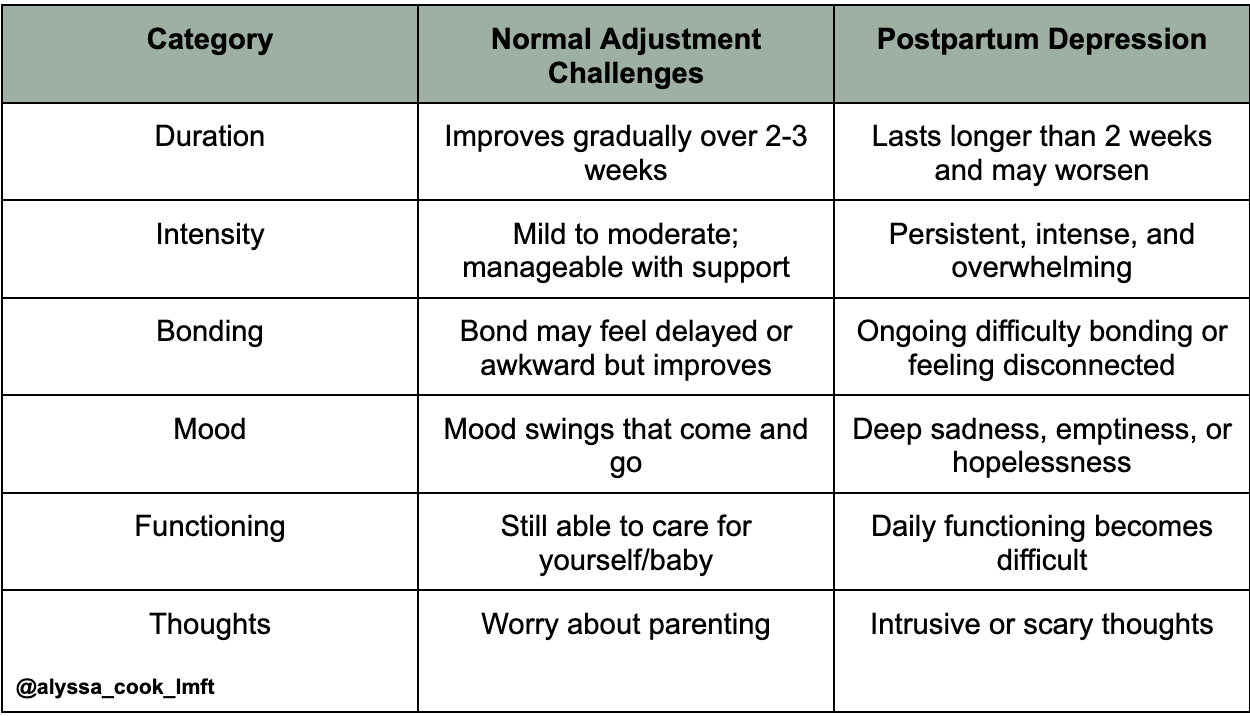
Key Differences: Normal Adjustment vs. Postpartum Depression
Here’s a simple breakdown to help illustrate the differences:
When Should You Seek Help?
If your symptoms:
last longer than two weeks,
interfere with daily functioning,
feel overwhelming or unmanageable,
or you’re experiencing intrusive or scary thoughts, it's time to reach out for help.
PPD is treatable with therapy, medication, support groups, or a combination of these.
Why Some People Are More Prone to PPD
There’s no single cause of postpartum depression, but risk factors include:
History of depression or anxiety
Traumatic birth experience
Lack of support from partner or family
Sleep deprivation
Hormonal sensitivity
NICU stay or medical complications
Previous pregnancy or infant loss
High expectations of self or perfectionism
Understanding these factors can help reduce shame and encourage early support.
How to Support Yourself Through Postpartum Recovery
Learning to care for yourself is essential, not selfish. Here’s how to support emotional health during the postpartum period:
1. Build a Support System
Accept help from friends, family, or postpartum doulas. Delegating tasks doesn’t make you less capable—it makes you human.
2. Prioritize Rest
Even short naps throughout the day can help restore emotional balance.
3. Connect with Other Parents
Support groups or parent-baby classes normalize the experience.
4. Lower Unrealistic Expectations
Your house doesn’t need to be spotless. Your baby doesn’t need a perfect routine. Good enough parenting truly is good enough.
5. Nourish Your Body
Hydration, balanced meals, and gentle movement can impact mood.
6. Create Moments of Self-Compassion
Use simple reminders like:
"I am learning."
"This phase is temporary."
"I deserve support, too."
When You’re Struggling: What Therapy Can Offer
Therapy can be incredibly helpful in the postpartum period, even if you’re not dealing with PPD. Working with a therapist gives you space to process identity changes, fears, relationships, and emotional overwhelm.
Therapists may use modalities like:
CBT to challenge intrusive thoughts
IFS to support overwhelmed internal parts
Mindfulness-based work to reconnect with the body
Emotion-focused therapy to process relationship shifts and communication
A therapist can help you build coping strategies, identify support needs, and reduce shame or isolation.
What About Partners?
Partners can also experience postpartum depression or anxiety, even without giving birth. Signs may include withdrawal, irritability, loss of interest, or feeling overwhelmed. The transition to parenthood impacts the whole family. Encourage partners to seek support if they’re struggling, you don’t have to navigate this alone.
Final Thoughts: You’re Not Failing, You’re Adjusting
Every parent experiences postpartum challenges. What you’re feeling doesn’t make you weak or inadequate, it makes you human. But if what you’re feeling goes beyond normal stress and starts impacting your ability to function, connect, or enjoy life, reaching out for help is one of the most loving things you can do for yourself and your baby. Postpartum depression is treatable, temporary, and nothing to be ashamed of. You deserve support, rest, compassion, and healing. If you're ready to talk to someone who understands postpartum mental health, I'm here to help you navigate this season with care and support.